Diastasis Recti – is there a “right” treatment?
It is Diastasis Awareness Month in July, bit late to the party but I’ve been swatting up on research papers around treatment. I’ve read 5 papers in the past week, many citing each other. While the nature of the papers vary in exact subject matter, they all agree on the following point. To quote the most recent surrounding treatment methods for Diastasis Recti (DR) (see end of blogpost for source):
“Although numerous studies confirm the positive influence of exercises on reducing the inter-recti distance no generally acceptable protocol of therapeutic exercises has been formulated so far. It has not been assessed which abdominal exercises are the most effective.“
“Taking into account still unsatisfactory knowledge regarding risk factors, possible consequences and effective methods of preventive treatment there is still a need of conducting further research in this field.”
Well this could be considered alarming especially given all the ready to buy DR fix programmes out there! And I could probably write a whole paper myself on all the findings I’ve come across within this research, but instead I’m just going to focus on a few points.
Firstly everybody is DIFFERENT. Everybody’s diastasis is DIFFERENT. And how they handle themselves day to day and during exercise is DIFFERENT.
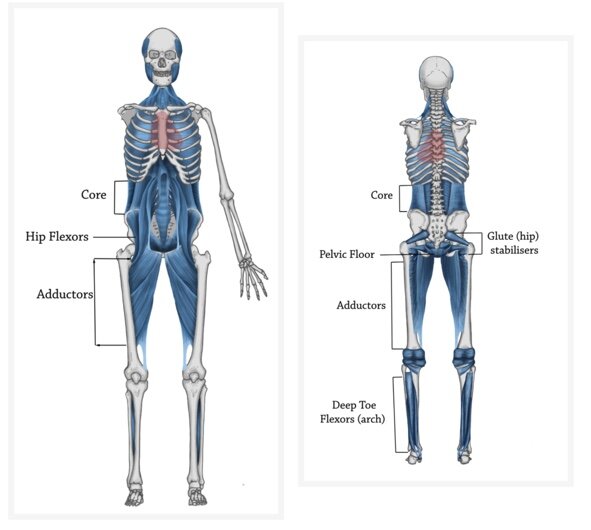
The whole body is connected so we need to think of diastasis as a total body issue from your feet to your head positioning (think Thomas Myers’ Anatomy Trains). It is not just about the core itself as important as this is. We do know that women with DR have a deep inner core unit that is not firing properly of course.
According to Lee and Hodges an abdominal curl-up results in the narrowing of the gap in most women however a pre-activation of the transversus abdominis (TA) muscle prevents the distortion of the Linea Alba (LA) i.e. firms up the gap or provides the tension.
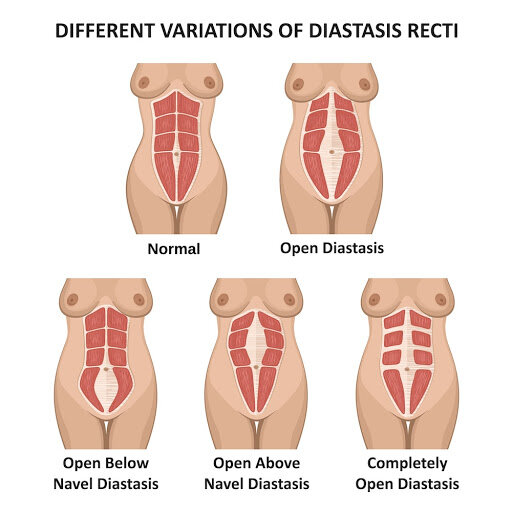
The optimal strategy and exercise prescription depends on YOUR DR e.g. are you wide but firm? How wide? Narrow but squishy? Both? Where is your opening – below, at the umbilicus, above, everywhere?
So where do you start? Identify the trigger, the route cause of the dysfunction which could include any of the following:
- Establish deep 360 breathing
You must be able to get a good inhale with lateral and back body expansion (not just belly) and exhale from the bottom up (ie. not bearing down). This increases natural pelvic floor and core functioning. You want balance in the system among the 4 respiratory muscles (diaphragm, pelvic floor, transversus abdominis and multifidus) and 4 core muscles (transversus abdominis, internal obliques, external obliques and rectus abdominis).
- Don’t forget about your pelvic floor!
You need strength in your pelvic floor to aid your TAs.
- Fix posture
And don’t forget about your ribcage angle when doing so i.e. fix rib flare which is so common postpartum. Look at everything from the arches of your feet to the angle of your neck. Even consider what your jaw is doing (clenching?) and tongue positioning during exercise!
- Work on abdominals
Work on how they are firing together, tension in the fascia (LA) and how you handle load (pressure control) in different positions during exercise or circumstances (daily life, picking up kids etc.)
- Check your diastasis in every position during exercise
What might be ok for you might not be for someone else and vice versa. Check for width, depth/tension and look for any doming/bulging/coning in the LA. Exclude exercises that make it worse!
Work with a specialist trainer (this doesn’t necessarily have to be me) or physiotherapist that can help and devise a programme for YOU. And if you do decide to go for an online programme, self/body awareness is key. Our bodies have an incredible way of cheating us into thinking we are performing exercises correctly. Film yourself, watch it back, identify your compensations and work (or learn) to correct. If you don’t feel you are getting anywhere, do seek out help.
Finally, DR is extremely common with pregnant and postpartum women. Please remember this. Mota et al. assessed the prevalence of DR at 35 weeks pregnant, 6–8, 12–14 weeks and 6 months postpartum. This decreased from 100% to 39.3% over the period. In another study by Sperstad et al. a higher percentage of DR occurred at 6 months postpartum at 45.4 %, decreasing to 32.6% at 12 months postpartum.
So please don’t be scared and be patient! Fascia does need SOME stress to heal (not too much to make DR worse of course) and it also needs time. In some ways we need to treat pregnancy like an injury. Our body has been through trauma and we should treat it with the respect it deserves. If any trainer says to you they can help you “bounce back” then I’d respectfully suggest you search elsewhere.
If you have any questions or want to book a consultation please do get in touch! rachel@rebornactive.com.
Article referenced source: Michalska, Agata & Rokita, Wojciech & Wolder, Daniel & Pogorzelska, Justyna & Kaczmarczyk, Krzysztof. (2018). Diastasis recti abdominis – A review of treatment methods. Ginekologia polska. 89. 97-101. 10.5603/GP.a2018.0016.